The [ Junior] Intern
I came into this year
thinking that I’m 1 year away from graduating, that it would be busy, fast
paced, and would pass by quickly enough.
Looking back on the past 8
months, I realized that I learned so much in such a short amount of time, but
also realized that I had so much more to learn.
These past 8 months, and 4
different rotations made me realize the following:
1. If you thought that you were tired, and you cant go on
anymore, youre wrong. There will always be that extra hour of energy to finish
that last few pieces of paperworks and cases.
2. There’s nothing that 10 billion cups of coffee and
energy drinks can fix on a long (very,very, very long) duty day.
3. Team work will be the only thing that can help you get
through toxic duty days.
4. There is an amazingly large difference between the
books/lectures and actual medical practice in the hospital. So when you see a
consultant/resident doing their rounds, jump up and join them.
5. Hardwork beats being smart anytime. But putting extra
effort in studying makes it extra better.
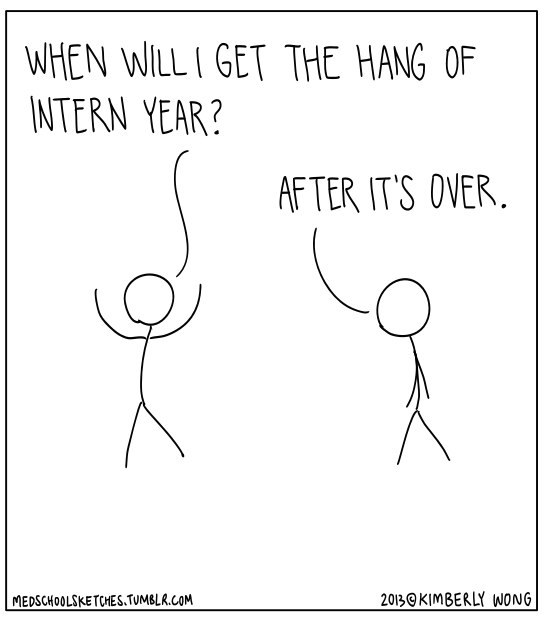 |
| http://medsketches.tumblr.com/post/60258641113/i-overheard-this-during-my-third-year-of-med |
6. Internship will break you, destroy you, harden you,
and then gradually build you up, make you, mold you, and turn you into the most
amazing, efficient intern ever [hopefully].
7. Internship teaches you the difference between working
with friends, and working with co-interns. Work is work.
8. You will constantly be amazed by the wonders of the
human body.
9. Situations such as sickeness and disease will show you
the best, and the worst in people in the hospital.
10. Medicine isn’t as glamorous as everyone thinks...
OB GYNE
This was probably the best
and worst time of my JIship. There is one thing that 3 years of med school wont
teach you and prepare you for—endurance.
Mental. Physical.
Emotional. Endurance.
This was like jumping off
a cliff into shark infested waters while you were bleeding.
The first month was
concentrated at the wards while the 2nd month consisted of special
rotations such as our rotation in GEAMH, OB Ultrasound, and OB Patho.
Que horror. That first
month was something I dreaded and hated to the fullest extent of my being. I
did not understand what I was doing since it was my first time to go on duty.
The concept of preduty, duty, post was foreign, and I really didn’t understand
what I was supposed to do as a clerk, coupled with extremely angry residents. I
understand their anger and confusion that their new JIs know nothing about OB,
and didn’t know how to actually present cases/ endorsements.
Everything was chaos every
day for the first few weeks and sleeping became a problem. I had constant
nightmares and remembered dreaming that I was on labor watch at the dorm. I
would find myself waking up with my hand propped up on a pillow imagining that
I was on labor watching, and wishing that she’d just undergo a CS instead.
The duties gradually
became better. I started to understand what I was doing. The topics became much
more understandable, and the stress levels were more manageable. But then
again, it still remained very difficult for everyone. The endorsements were
brutal. These 8am meetings at the SGD were absolutely brutal, and you just
wished that you never had been decked with patients. I was lucky that my
resident buddy was the best, and would teach me a few minutes before
endorsements just so that I wouldn’t be tortured in front.
The worst moment of OB was
during my post duty, and one resident as looking for two more junior interns to
assist in their TAHBSO. The patient was a 36 year ol female, nulligravid, and
was to undergo TAHBSO for the presence of her Ovarian New Growth. She had a BMI
of more than 30. At first, I just thought that that was an extremely large
patient. What i didn’t know was the extent of these small details about the
patient which would affect the outcome of the operation. The resident was scary
as hell, and kept asking me if I would still be able to retratct considering I
was post duty, and had such a horrible duty. I wanted to prove myself to her,
and confidently said yes. During the operation, we spent 1-2 hours trying to
cut through the thick layer of fat which contributed to her amazing BMI. Two hours into the operation, the post duty
syndrome was really kicking in, I was struggling to stay awake, and retracting
is by no means an easy task. I felt destroyed when the resident called in
another JI to help out. Althroughout the operation, the resident kept shouting
at me, telling me that the only job I had was to retract, and I couldn’t even
do it right. An hour later, I was really tired and demoralized, and the
resident could sense it. She asked me to scrub out, but I was trying to really
prove myself. The resident kept telling me to scrub out, and in the end, the
senior intern asked me to go instead of making it difficult for everyone. I
scrubbed out. I felt down. But somewhat relieved. I went home, slept for 20
hours straight, with a heavy heart. The following day I learned from my duty
mate that the operation lasted for 10 hours...and that the chief resident gave
the JI and I a 24 hour merit for good patient care. I felt so happy for it, but
at the same time, felt undeserving. It was a minor thing to happen, but for
some reason, it had such an impact on me.
COMMED
Commed was the rest and
relaxation that everyone was looking forward to. It was definitely worth it,
but it wasn’t what we expected. We were stationed in Kabulusan, and the houses
were far apart from each which didn’t give us enough bonding time with each
other unless its breakfast, lunch, merienda, dinner, or patient visits. The
experience was wonderful and was a welcome relief from the harassment of a
rotation called OB.
During our rotation, we
rotated in the OPD, TB DOTS, and the community immersions. TB DOTS wasn’t much
of a learning experience since the rains kept getting in the way, resulting in
multiple cancellations of classes. We spent only half a day at the TB DOTS, and
we weren’t able to even give any medications to any of the patients since it
was all done.
The OPD was probably the
toughest OPD I had ever experienced. The histories and case files were long and
winding, the patients mostly elderly with very very complicated and vague
histories that no amount of time could straighten out, and the big surprise
factor in every day at the OPD.
One of the most memorable
moments was at the OPD, and the patient had the same birthday as me. He was
covering up his left eye with a towel, and at first, we all thought that he
should be sent to the Surgery Department for trauma. Upon asking him to take
off the towel, I saw ptosis of the left eye, and a non reactive pupil, while
the other eye was perfectly fine. I still didn’t know what to diagnose the
patient, since it was my first time exposed to another case other than OB. I
asked help from my senior interns and they just kept commenting that “ang toxic mo”. The chief resident who
was the whole thing from afar barked out that I should do a full PE on the
patient, complete with neuro exam. I thought that it would be entirely
different from the OB PE, and assumed he was asking for the complete PE
similarly done in the 3rd year, with complete skin, ENT, abdomen,
etc findings, complete with special maneuvers, and 3 senior interns were
already helping me out so I assumed that what we were doing was correct. An
hour had passed when I still wasn’t finished with the PE, and included was the
medical abstract which I had no idea how to do since it was my first time. The
patient was sent to another hospital for transfer, and what surprised me was
the patients’ discharge diagnosis, it was a case of stroke. Call me a little
ignorant, or unknowledgeable but there is a huge difference between how the
books describe it, and seeing it in real life. I was completely horrified. The
resident called me, along with my senior interns, and started shouting at me.
He went on for 5 minutes, telling me how slow I was, that I was taking it
seriously, and that I did a poor job of handling the patient. I felt
demoralized since he was shouting at me, in front of everyone. He then
explained (but still angry) that the only reason why he kept rushing and
harassing me was that the patient needed immediate attention, was in a
post-stroke time frame, and may develop into another stroke. It was only then
that I realized how bad I handled the situation. I brooded over the occurrence
the whole week, and then accepted that that was going to be the only way I
would learn.
MINORS
OPHTHALMOLOGY
Ophtha was suprisingy fun,
and its a specialty that seems to be taken for granted in my opinion. The OPD
was confusing, and difficult, with so many tests being done.
ER was equally fun due to
the sore eyes epidemic that spread during that time. There was one duty (not
mine though), that they had 30 ER calls, 90% of them were sore eyes, whole
families, classmates, relatives, and what really frustrated me was that they
would come in at dead hours of the night. I mean, any sane being would rather
rest it and go to the clinic or hospital in the morning when they were more
rested. These people would come at 2am and would be agitated that it would take
so long for us to process them since it was in the wee hours of the morning.
ORTHOPEDICS
I didn’t expect Ortho to
be sa tiring and difficult, and gross. It really made me squirm to see twisted
legs, ankles, broken bones, fractured ribs and the like. On inital management
of the patient, it would require you to splint the affect extremitiy, but it
seemed like we always made it worse. There was an abundance of diabetic foot
cases, fractures, and ingrown toenails. At the OPD, we got to participate in an
ungiectomy, as it was my first time seeing one. It was absolutely gross, and
the whole toe nail was actually pulled off! I promised myself that after this
rotation, I would take better care of my feet, and would never want to have anything
done, or any procedure done at all.
PSYCHIATRY
This was probably the
weirdest rotation I had. JIs who rotated here were usually benign, but during
one time, I was decked with a patient who tried to commit suicide because her
husband was engaged in an accident, and had to undergo an ORIF, but was unable
to due to lack of funds. She had taken a kitchen knife, and tried to stab her
mother in law, and then herself, by stabbing herself in the abdomen. She
underwent an emergency ex-lap and was put on suicide watch for the next few
days where we had to do a q6 MSE.
Another memorable event
during my psych rotation was our trips to CCMH. These mini experiences at the
center were shocking, and sometimes vulgar. The patients were mostly
schizophrenic, a few were depressive, some were psychotic. At first, I had no
idea how to manage these type of patients, but through time, we got the hang of
it. It was during this time that we were assigned to different consultants for
our oral exam with them...and guess who I got? Dr. Dejamco. The Dr. Dejamco.
I had never seen her. For
the past two courtesy calls that we tried to do, she absolutely refused to meet
us, and sent her secretaries to talk to us, give messages, and schedules for
the exam. By our last duty there, I was completely horrified. There were two of
us and she decided to do the oral exam at the same time. I was expecting a
hurricane of an exam, but surprisingly , she asked basic questions that were
never taught at school, basics such as doing an MSE, history taking,
understanding schizos and their cases. We were able to answer most of the
questions, and after an hour of intense grilling, she asked us to step out, so
she could grade us. A fewminutes later, she handed us our grading sheets, and
surprise, surprise! She gave us 13/15, the highest that she had gven so far to
any Lasalle JI. The rest we heard from had been given 8/15, and the like,
barely passing. I thought it was a huge
achievement for being able to get such a grade.
Because.we.had.conquered.Dejamco.
ENT
QUE.HORROR. This rotation
was horrible. OB was better than this. The residents were difficult ,
one made me cry and demoralized me in front of the whole group, the patients
were all difficult, crying, bleeding from the mouth or nose, with batteries,
coins, and cotton buds stuck everywhere. One case that really frustrated me was
a 2 year old baby, brought in at 3am by the mother and father, complaining of
bleeding from the ear. Upon history taking, she was cleaning her son’s ears
when he was playing around with buds, pretending to be a robot/Frankenstein.
First off...why are you cleaning your sons ears at 3 in the morning? And all of
them are in such a bad mood since we had difficulty checking his ears, and the
patient became very agitated.
At times like these, I
question these parents and what they do in the wee hours of the morning. They
are angry at you for advising them on the proper ways of cleaning ears, proper
hygiene, proper safety procedures, but when harm comes to their child, they lay
no blame on themselves for the occurrence.
I dreaded the 15 days of
my rotation there, I didt enjoy it at all, and it is one of the rotations that
Im dreading for this upcoming SIship.
ANESTHESIA
Our chosen elective was
the bomb. It was such an eye opener, and I enjoyed every minute there. It came
to the point that I put it up on my list of possible specialties for my
residency. I never thought it would be so interesting and action packed to be
looking at a few monitors, and seeing so many cases within the day. It was
every bit exciting to see different consultants have different techniques in doing anesthesia.
INTERNAL MEDICINE
This was by far, the most
challenging rotation ever. I would rather repeat OB than do IM again. The cases
were neverending, the paperwork was frustrating to do, with demanding
relatives, and demanding nurses, and demanding everything. The cases were a mix
of benign and toxic. It was during this rotation that I experienced my very
first mortality.
He was DB, 65 years old,
with a history of DM, and had suffered from Uremic Encephalopathy. He came in
already with decreased sensorium, he smelled uremic too. I thought that
perhaps, he would get better once he underwent hemodialysis or something. We
spent the whole night, q1, making sure he was doing better. I breathed a sigh
of relief upon my post duty status, with him still alive, and semi-well. While
preparing my papers for the duty, I heard the heart stopping announcement. Your attention please, your attention
please. Code blue, code blue, 1400. Code blue, code blue, 1400. I
immediately knew it was my patient. I ran across the floors, and bypassed
everyone, jumped on the bed, and started resuscitating the patient. 1 epi, 2
epi...10 epis later, and he was then pronounced dead.
I wanted to cry, but I
didn’t. It would have been unprofessional. I don’t know wjy, but for some
reason, his death affected me so much. I would not forget this patient ever. He
would serve as a reminder of how much I needed to study some more, to be able to
treat my patients.
SURGERY
Pretty much like OB and
Commed, Surgery was the Commed of that time. Although it was toxic, in terms of
the emergency Ors, the monitoring was by the most challenging thing to do. It
was tiring. It was smelly, and it was messy to do most of the time. The ORs
were long, and for me, boring since I couldnt see much of the operating field. I couldn’t see much, and the residents were very
stressed and concentrated on their work, so you couldn’t really bother them
that much about the speicifcs of the case. It was during this time that I
realized that I didn’t want to go into Surgery at all.
It was fun, and exciting and all, but it wasn’t for me. The cases I had consisted mostly of chornic calculous cholecystitis and appendicitis, and in the first few weeks, was exciting, but then it grew to a point that I had lost interest already. I know its kind of wrong to feel this, and that everything is a good opportunity to learn, and that every case was different, but I really had some difficulty trying to keep up the motivation.
It was fun, and exciting and all, but it wasn’t for me. The cases I had consisted mostly of chornic calculous cholecystitis and appendicitis, and in the first few weeks, was exciting, but then it grew to a point that I had lost interest already. I know its kind of wrong to feel this, and that everything is a good opportunity to learn, and that every case was different, but I really had some difficulty trying to keep up the motivation.
PEDIATRICS
Everyone. And I mean
everyone had warned me over and over about how horrible it was. We would be
reduced to being monitoring machines. Learning would come every so often, and
interesting. So far, it wasn’t as bad as I thought it was.
OPD was the most amazing
thing. Im not saying it because of the schedule, but the learning there was immense.
The one on one with the mothers, and their babies,was amazing. The educating
the mothers on new practices, and correcting them on their most common
misconceptions was entertaining because of how the mother and their
grandmother’s practices were constantly clashing. The patient had dermatitis
with superimposed bacterial infection. Instead of using cetaphil soap and the like, she put her own
breastmilk on the babies face, saying that her neighbours advised her to do so
since it was nutritious, and was like any other milk bath, that would help
soothe inflamed skin. It was frustrating at first, but upon educating the
mother, she realized how foolish it all seemed.
ER was the next best
thing, the most action packed, and the most difficult. The patients weren’t the
problem. Most of it the time, it was the relatives, mother, father, and the
most notorious of them all, their lola, that made the whole situation
unbearable and difficult. It was a good thing that our resident was extremely
patient, and gave us the extra support we needed.
The wards was an entirely
different thing all together. The work was monotonous, the hours long, and the
monitoring was difficult with pediatric patients. On my first duty, I was
assigned to bedside of a new case, a 33 week old neonate, who was suggested to
have Down’s Syndrome, to consider Edward’s Syndrome, with pleural effusion,
neonatal sepsis secondary to neonatal pneumonia, and now was being considered
for hydrops fetalis. She was on mechanical ventilator, and had episodes of
desaturation that made the monitoring all the more difficult. For the next two
days, she was monitored closely, and I began to grow fond of her. By my last
duty, I came in and found the room empty. I was completely surprised, and my
heart pounded thinking that something bad had happened to her. On endorsement,
I found out that she had self extubated herself, and was breathing fine on her
own. Her parents had already signed the DNR waiver, and HAMA, thinking that if
she were to pass early, at least it would be at home, without debt. I seriously
hope that I wont see her again in the hospital unless its for a well baby
checkup.
OVERALL
Im just glad JIship is over.
I'd give it a score of 100/100. Hahahahahaha
But Im definitely dreading senior internship.
and the boards.
Oh well.
No comments:
Post a Comment